Dawn Gideon Symposium
The Dawn Gideon Symposium is an annual educational event funded by the Dawn Gideon Foundation, conducted by the Department of Health Policy and Management in cooperation with the HPM Alumni Association. This symposium is Grand Rounds eligible.
2024 Event
If Not Now, When? The Challenges We Must Face Providing Mental Health Services in Today's Aging Society
Moderator: Marty Raniowski, MPP, (UPJ ‘93)
Raniowski is chief executive officer of the Pennsylvania Medical Society. His professional career spans two decades, with experience in state government, academia, health non-profit, client-based research and association management. He has a distinguished career in health care policy, with his previous position being deputy secretary of the commonwealth PA Department of Health.
Panelists: Ellen Whyte, MD, Dale Adair, MD, DLFAPA, Deborah Brodine, MHA, MBA

Ellen Whyte is the assistant professor of psychiatry, physical medicine and rehabilitation at Pitt Medicine. She is the clinical chief of geriatric psychiatry; medical director of the UPMC Western Psychiatric Hospital’s Geriatric Psychiatry Ambulatory and LTC Services as well as medical director of WPH’s Integrated Behavioral Health in Primary Care Program. She received her MD from the SUNY-Buffalo School of Medicine and Biomedical Sciences, completed a residency at University Hospitals of Cleveland and a fellowship and postdoctoral work at UPMC and Western Psychiatric Hospital.
Dale Adair is the Pennsylvania Department of Human Services (DHS) Chief Psychiatric Officer and the Medical Director for the Office of Mental Health and Substance Abuse Services (OMHSAS). He provides clinical expertise and consultation to the Deputy Secretary of OMHSAS and the Secretary of DHS. He has been a leader in the development of the vision for PA’s First Episode Psychosis program; PA team efforts with the Center for Medicare and Medicaid Innovation Accelerator-Substance Use Disorder project; Centers of Excellence for the treatment of Opioid Use Disorder; Health Equity; and served as project lead for the PA Certified Community Behavioral Health Clinic Program. Most of his career has been spent addressing the mental health concerns of the most vulnerable citizens. He is a distinguished life fellow of the American Psychiatric Association.
Mental Health and Substance Abuse Services (OMHSAS). He provides clinical expertise and consultation to the Deputy Secretary of OMHSAS and the Secretary of DHS. He has been a leader in the development of the vision for PA’s First Episode Psychosis program; PA team efforts with the Center for Medicare and Medicaid Innovation Accelerator-Substance Use Disorder project; Centers of Excellence for the treatment of Opioid Use Disorder; Health Equity; and served as project lead for the PA Certified Community Behavioral Health Clinic Program. Most of his career has been spent addressing the mental health concerns of the most vulnerable citizens. He is a distinguished life fellow of the American Psychiatric Association.

Deborah Brodine is the president of UPMC Western Psychiatric Hospital and the Western Behavioral Health Services line of UPMC. She has more than 30 years of progressive, strategic leadership in healthcare. She has depth of experience in population health strategies that cut across multiple levels of care, and that require engagement with both payers and providers. Brodine has a wealth of experience in implementing collaborative programming including the formation and ongoing support of joint ventures, management services agreements and community engagement initiatives.
Past Symposia
- 2023 Lecture - Rural Health at a Crossroads: Reinventing for the New Economy
For many citizens, losing the local hospital would threaten the livelihood of the town's economy and its people. Although rural health systems face what traditional hospitals experience, they have a smaller, often more vulnerable population to support operational expenses. Handling supply chain disruptions, workforce burnout, and managing financial losses while maintaining clinical quality is especially challenging as rural facilities determine how to return to pre-pandemic profitability while unit costs continue to increase. But many have discovered innovative solutions like partnering with nearby critical access facilities, operating mobile clinics and pursuing grant opportunities. Join our panel experts as they discuss the challenges to sustain these hospitals, including how they address limited funding, regulatory restrictions, problems with transportation and internet accessibility while continuing to provide quality care as a priority.
Moderator & Panelists

Marty Raniowski Moderated by Marty Raniowski
Executive Vice President and Chief Executive Officer, Pennsylvania Medical SocietyPanelists
Lisa Davis
Director, Pennsylvania Office of Rural Health
Outreach Associate Professor of Health Policy and Administration, Penn StateAndrew Watson
Professor of Surgery and Senior Medical Director, UPMC Health Plan
Senior Medical Advisor, UPMC EnterprisesSteve Wolfe
President and CEO
Indiana Regional Medical Center


Lisa Davis ensures that the Pennsylvania Office of Rural Health exceeds its mission of being a source of networking, coordination, and technical assistance to advance rural health care delivery. On national, state and university levels, she serves on a wide range of boards of directors, advisory committees and task forces focused on rural health policy, rural health research, economic development, outreach and education, vulnerable populations and specific health issues such as oral health and cancer.
Davis is the recipient of the Distinguished Service Award from the National Organization of State Offices of Rural Health, an Outstanding Leadership Award from the Pennsylvania Rural Health Association, and an Award for Individual Contributions to Public Health from the Pennsylvania Public Health Association. The Pennsylvania Office of Rural Health received the Award of Merit and the Award of Excellence from the National Organization of State Offices of Rural Health.
Andrew Watson is a fourth-generation surgeon and the eighth surgeon in his family. He earned his master's degree at the University of Oxford and attended medical school at the Columbia University College of Physicians and Surgeons. He did his surgical training and fellowship at UPMC. He is an actively practicing colorectal surgeon specializing in minimally invasive inflammatory bowel diseases and complex re-operative abdominal surgery. He is a professor of surgery and works within the division of colorectal surgery. Watson is widely published and recognized as a telemedicine expert.
Watson spends the majority of his time working for corporate UPMC. He is the senior medical director for digital health at the UPMC Health Plan, focusing on digital health and strategy for Health Plan members. He is a senior medical advisor for UPMC Enterprises focusing on digital health innovation and investment opportunities. He is also a senior medical advisor for UPMC International and focuses on telemedicine and access.
He actively uses and helps to develop telemedicine at UPMC and has personally conducted over 800 telemedicine visits for pre- and post-surgical patients. He is past president of the American Telemedicine Association and an advisor to the American Board of Telehealth.
Steve Wolfe is the current president and CEO for Indiana Regional Medical Center (IRMC). Under his leadership for more than 20 years, there has been significant turnaround of IRMC's performance and results in its five organizational vitals: finance, service, quality, growth and people. The leadership team has led the organization's growth of approximately 250%, consistently achieved top decile national outcomes for quality and service metrics, been voted a best place to work 15 times by employees and physicians and achieved a national goal of being named to the Fortune 100 List.
Moderator Marty Raniowski is the executive vice president and chief executive officer of the Pennsylvania Medical Society, the largest physician-run association primarily focused on state-level health issues impacting Pennsylvania physicians and their patients. It consists of about 17,500 physicians, physicians-in-training and medical practice administrators from across the Commonwealth.
Raniowski's professional career spans two decades of experience with state government, academia, client-based research and association management. He has a distinguished career in health care policy, including a position as deputy secretary of the Commonwealth of Pennsylvania Department of Health (DOH). During this time, he provided leadership for staff working to implement statewide health plans. Among some public health disasters and threats that he addressed during his tenure were Hurricane Irene, Tropical Storm Lee, Superstorm Sandy, and Ebola. Prior to advancing to deputy secretary, Raniowski began his career with the state as director of health planning in 2007. As an association professional, he served as senior director of public advocacy with the American Heart Association's (AHA) Pennsylvania/Delaware Affiliation, where he worked with numerous partners to promote AHA initiatives including quality improvement in primary care and hospital settings. His career in government also includes positions with the Pennsylvania House of Representatives Health and Human Services Committee and the Governor's Chief of Staff's Office.
- 2022 Lecture - The Parallel Pandemic: Impact on the Workforce
Moderated by Marty Raniowski
Executive Vice President and Chief Executive Officer, Pennsylvania Medical SocietyPanelists
Ritu Thamman, M.D., FACC, FASE
Assistant Clinical Professor of Medicine, University of Pittsburgh School of Medicine
Buffy Kelly
Managing Director, Huron Consulting Group
Kimberley Finnerty
Nurse and VP of Workforce Planning, Highmark

About Our Presenters
Kimberley Finnerty is the Vice President of Workforce Planning, Financial Operations, for Allegheny Health Network (AHN). Kimberley’s responsibilities include planning, developing, and evaluating enterprise-wide strategic staffing to ensure timely and high-quality patient care. Kimberley works closely with the Senior AHN Executive Leadership team, as well as the executives in the finance and operational areas. Kimberley often collaborates with multidisciplinary teams, which ensures the integration of care expectations in operational business units, as well as the equitable allocation of workforce resources across the network. Kimberley allocates workforce resources based on patient acuity and care need, develops business unit models, participates in business unit workflow projects to enhance staffing efficiencies, and leads network and hospital-level workforce planning initiatives through identified tactics and in collaboration with established committees. Kimberley and her team collect, collaborate and analyze internal and external workforce data, trends, analytics, and insights to assess gaps, and prioritize risks and opportunities. They also design key elements of operational and financial dashboards related to workforce management and financial operations. In addition, she reports workforce planning information related to business operations, budget analysis, productivity management, operational analytics, contingent labor contracting and analytics. Kimberley was key in staffing the Covid Vaccination Clinics hosted by AHN.
Kimberley has worked with AHN for the last sixteen years serving in multiple leadership roles. Prior to AHN, she worked at the University of Pittsburgh Medical Center. She graduated from Duquesne University and has been a Registered Nurse for 25 years. Kimberley is also a major in the United States Air National Guard. In 2000, she received the prestigious Cameo of Caring Award. She is also the current President of the West Jefferson Hills School Board, as well as a Chairperson for the Steel Center Vocational School Executive Advisory Board. Kimberley enjoys spending free time with her husband and three boys in the South Hills area.
Dr. Ritu Thamman is an Assistant Clinical Professor of Medicine at the University of Pittsburgh School of Medicine. She is a writer and the co-course director for Narrative and the Experience of Illness at the University of Pittsburgh School of Medicine. She is also part of the Health Humanities faculty at the Center for Bioethics and Health Law at the University of Pittsburgh. Her book on the prevention of burnout in medicine was published in 2021. The following year she received the Carl R. Fuhrman Clinical Educator of the Year from the School of Medicine. Dr. Thamman started the Women in Cardiology Chapter PA ACC in 2018 and her writing and interpretation of scientific articles have led to her being a top social media figure for advocacy and education.
Buffy Kelly has over 25 years of healthcare and consulting experience which began in the clinical laboratory. She is also highly skilled in the operations and optimization of workforce management and patient flow throughout hospital and ambulatory settings. Buffy’s other areas of interest focus on management structure redesign, including op model re-design/span of control, operational improvement, outsourcing and facilitating organizational change. She has extensive experience working in union environments.
Buffy grew up on a cattle ranch in Wyoming, played college volleyball at Eastern Wyoming College and graduated from the University of Wyoming with a degree in Medical Technology. She began her healthcare career working in the laboratory at a 25-bed critical access hospital in rural Wyoming where she gained experience working in rural medicine. Buffy owned a consulting firm before joining Huron and consulted with clinical and anatomical laboratories in 60 healthcare systems across the country to improve efficiencies, optimize staffing and technology and provide system consolidation guidance.
Buffy continues to live on a working cattle ranch in Wyoming with her husband of 25 years, Clay, and their two children Rachel (22) and Chance (19) who are both students at the University of Wyoming. Buffy is also a professional photographer and enjoys golfing and traveling in her free time.
- 2021 Symposium - Covid-19 - Challenges Faces, Lessons Learned, Moving Forward
Monday, November 8, 2021
1-2:30 p.m.Moderator
Marty Raniowski, Executive Vice President and Chief Executive Officer
- Pennsylvania Medical Society
- Anita J. Tarzian, Deputy Executive Director, National Center for Ethics in Health Care
Panelists
Amy Cashdollar, Chief Operating Officer, Allegheny Health Network, Wexford Hospital Michael Morley, Associate Partner, McKinsey and Company
- 2020 Symposium - How COVID-19 is Changing the Virtual Health Care Culture: Access, Experience, an Financial Incentives
Monday, November 9, 2020
1-2:30 p.m.Decades prior to the COVID-19 pandemic, health care systems around the globe were actively engaged in thoughtful design, refinement, and implementation of smart solutions to address patient flow, access to quality care, and operational management. While many innovative solutions were in place or previously proposed at various levels in health care administration and delivery, the pandemic forced patients, providers, and payers to shift to virtual health applications seemly overnight. Our expert panelists working in the field will discuss the far-reaching effects that COVID-19 has had on virtual health care culture—including lessons learned—to provide a framework for solutions addressing access, experience, and financial sustainability.
Moderator
Angela Perri, Vice President, Strategic Alignment, Transformation & Consumer Innovation, UPMC Health Plan
- Larry Stuckey, Managing Director, Huron Consulting Group
Panelists
Tom Priselac, President and CEO of Cedars - Sinai Health System Chris Johnson, President of TeleTracking Technologies, Inc.
- 2019 Symposium - Reading the Sign Posts: How Healthcare Organizations are using Social Determinants of Health to Address Health Disparities
Monday, November 11, 2019, University Club, Ballroom B
Noon luncheon and arrival
1:00 p.m. lecture and webcast portion of the program
2:30 p.m. meet and greetModerator
Ebbin Dotson, Assistant Professor of Health Management and Policy, University of Michigan School of Public Health
Tweet and Tag #GIDEON @PITTPUBHEALTH
Panelists
Melinda Buntin, PhD, Mike Curb Professor of Health Policy and Chair, Department of Health Policy, Vanderbilt University School of Medicine Maureen Hydok, RN, MBA, Healthcare Senior Director, Huron Consulting Group Thuy Bui, MD, Associate Professor of Medicine; Director, Social Medicine Fellows Program, University of Pittsburgh School of Medicine
- 2018 Symposium - Innovation Impact: Collaboration, Consolidation, and Competition in Health Care
Innovation Impact: Collaboration, Consolidation, and Competition in Health Care
Monday, November 12, 2018, University Club, Ballroom A
Noon Luncheon and arrival
1:00 PM lecture and webcast portion of the program
2:30 Meet and greetModerator
Everette James, M. Allen Pond Professor of Health Policy and Management; director, Health Policy Institute, University of Pittsburgh
Hear senior health care leaders explore how organizations are adopting innovative strategies to survive and prosper in the new environment. Experts answer your questions on innovations in technology, service delivery, and organizational change.
- Rasu Shrestha, chief innovation officer, executive vice president, UPMC Enterprises
Panelists
Sarah Ahmad, senior vice president, innovation and transformation strategy, Highmark Health Lou Shapiro (HPM ʼ85), president and chief executive officer, Hospital for Special Surgery
- 2017 Symposium - Tackling the Social Determinants of Health: The Next Big Challenge in Health Care’s C-Suites
Monday, November 13, 2017; University Club, Ballroom A
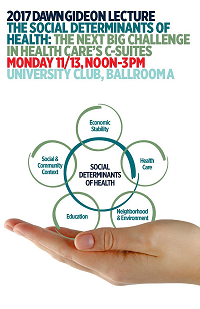
How and why must the nation’s leading health care organizations address the social determinants health in their corporate strategies?
Hear from former president and CEO, ROBERT HENKEL (’83), how Ascension Healthcare plan to achieve—by 2022—zero preventable health care disparities across the continuum of care.
Then get a broader perspective on how management must evolve to efficiently and equitable address population health from a reactor panel that includes:
Mike Blackwood (’80) former president and CEO of Gateway Health, Marian Jarlenski, assistant professor of health policy and management, and GARY PERECKO (’81) president of Main Line Health System’s Riddle Hospital.
View 2017 Program (pdf)
Tweet and tag #Gideon @PittPubHealth- 2016 Symposium - Health Care’s Newest Code Blue: The Need for Cash Infusion and Restructuring!

Monday, November 14, 2016; The William Pitt Union BallroomThe health care industry is one of the most turbulent industries in this country. It consumes the largest percentage of GDP of any industry, and has resulted in both tremendous fortunes and business failures. Regulations and reimbursement methods have become very diverse and complex, and these affect both the financial and clinical performance of health care organizations. Every year, one or more segments of the health care industry cycles through a restructuring for various reasons. This panel will explore why there is so much turbulence in the industry and whether there is any way to improve the prospects of a health care business’s success amid all of these challenges. The speakers will explore...
The key drivers of operational and financial performance in this industry; The government’s enormous impact on the success or failure of the healthcare business by exploring ongoing increases in government regulation, ongoing changes in reimbursement rates, fraud issues, and the impact of qui tam actions; The unique challenges of turning around a non-profit entity and the restrictions on restructuring options for such non-profits; Whether there is really any way to turn around a healthcare business heavily dependent on Medicare and Medicaid funding; and Whether investors should be putting their capital to work in this industry.
2:30 Audience Q/A
3:00 Adjournment
View the Webcast video or download the program booklet (PDF).
2:00 Alumni Reactor Panel
David Hunter, past managing partner, Hunter Partners Robert Henkel, president & CEO, Ascension Health; executive vice president, Ascension Michael Young, president & CEO, PinnacleHealth System
- James Nugent, managing director, Huron Consulting Group
- Nancy Peterman, chair, Chicago Business, Reorganization & Financial Restructuring Practice, Greenberg Traurig, LLC
12:30 Invited Speakers
Suzanne Koenig, president SAK Management Services, LLC
Agenda
11:30 Arrival
11:45 Lunch Buffet
12:15 Welcome
Mike Evans, president, HPM Alumni Association Mark Roberts, professor and chair, Department of Health Policy and Management
Sonis Lecture
For more than 20 years, The Sonis Lecture has stood as HPM’s premier annual event focusing on health care quality and safety. It is sponsored by the family of Anne C. Sonis, the Pitt Public Health Department of Health Policy and Management, the Wolff Center at UPMC, and the UPMC Health Plan. It is also part of the Dr. Loren Roth Quality and Patient Safety Speaker Series of UPMC.
This event is Grand Rounds eligible and provides AMA PRA Category 1 CME credits for physicians and AAPA Category 1 CME credits for physician assistants.
2025 Sonis Lecture
Maternal Mortality in the U.S.: Myths, Legends, and Lifesaving Truths
Presented by Aasta Mehta, MD, MPP
Director, Division of Child, Family and Maternal Services, City of Philadelphia Department of Public Health
Thursday, March 13
Learning Objectives
- Examine fundamental concepts of maternal mortality
- Analyze current national and local maternal mortality data
- Debunk myths surrounding maternal mortality in the U.S.
- Present key findings and the influence of obstetrical care on outcome enhancement
- Read more about Mehta
In Aasta Mehta’s role as director of the Division of Maternal, Child, and Family Health (MCFH) at the Philadelphia Department of Public Health, she oversees all aspects of the city’s maternal and infant health services, including the development and implementation of program policies, service standards, grant and strategic planning efforts, and the evaluation of provider services. Mehta leads efforts to ensure high-quality, equitable care for Philadelphia’s mothers, children, and families through a comprehensive approach that includes direct services, contracted providers, and innovative public health initiatives.
Under her leadership, MCFH manages citywide programs such as maternity services, family planning, infant care, outreach efforts, home health services for high-risk infants, and support for women experiencing substance use disorders or intimate partner violence during pregnancy. Mehta also guides the division’s advocacy efforts, working with legislators, governmental officials, and community stakeholders to shape policies and secure resources that address health disparities and promote healthy behaviors among families.
As part of her role, Mehta directs the Philadelphia County Maternal Morbidity and Mortality Program (Birth Justice Philly) and collaborates with state and local organizations as co-chair of the Pennsylvania Maternal Mortality Review Committee and the Pennsylvania Perinatal Quality Care Collaborative Advisory Group. She oversees the formulation of medical policies, program evaluation systems, and interagency agreements to establish an integrated citywide maternal and infant health network.
Mehta is also a practicing OB/GYN hospitalist at Penn Medicine, where she provides comprehensive care to patients and remains directly engaged in clinical practice. She brings this hands-on experience to her public health leadership, ensuring a practical and patient-centered approach to policy and program development.
In addition, Mehta serves as affiliate faculty at Drexel University's Dornsife School of Public Health, where she developed and teaches a course on problem-solving to improve maternal health. Known for her data-driven and equity-focused approach, she has developed innovative solutions to reduce maternal and infant health disparities and improve public health outcomes.
Mehta completed her residency in obstetrics and gynecology at Drexel University College of Medicine/Hahnemann University Hospital and earned a master of science in public policy from Drexel University, specializing in health policy.
Past Sonis Lectures
- 2024 Sonis Lecture
Can Health Care Learn at Scale? From Sepsis to AI: Promise and Pitfalls

Tuesday, March 5, 2024
3-4:30 p.m.
University Club, Ballroom BPresented by Vincent Liu, senior research scientist at the Kaiser Permanente Northern California Division of Research.
Learning Objectives
Health system approaches to improving sepsis care Identifying opportunities to apply learning health system principles in routine health system care
- Understanding the role that artificial intelligence may play in enhancing the learning health system
- 2023 - The National Healthcare System Action Alliance to Advance Patient Safety: Improving Patient and Healthcare Workforce Safety
The National Healthcare System Action Alliance to Advance Patient Safety: Improving Patient and Healthcare Workforce Safety
Keynote Speaker
Robert Otto Valdez, director of the Agency for Healthcare Research and Quality

About
Robert Otto Valdez, was appointed director of AHRQ in February 2022. He was previously the Robert Wood Johnson Foundation Professor Emeritus of Family & Community Medicine and Economics at the University of New Mexico. He received his PhD from the Pardee RAND Graduate School for Public Policy Studies specializing in studies of health care financing and quality of medical care. At the University of Michigan School of Public Health, he was awarded a master of health policy and administration. At Harvard University, Valdez studied in the Department of History and Science specializing in Latin American history and biochemistry.
- 2022 - What Does a Learning Health System Really Mean?
What Does a Learning Health System Really Mean?
Tuesday, March 22, 2022
View Webcast »Keynote Speaker
 Derek C. Angus, MD, MPH, FRCP
Derek C. Angus, MD, MPH, FRCP
Associate Vice Chancellor for Health Care Innovation, Health Sciences
Distinguished Professor, Mitchell P. Fink Professor, and Chair of Critical Care Medicine, Professor of Medicine, School of Medicine
Professor of Health Policy and Management, Graduate School of Public Health
Professor of Clinical and Translational Science, University of Pittsburgh
Executive Vice President and Chief Innovation Officer, UPMCAbout
Derek Angus is executive vice president and chief innovation officer at UPMC. He oversees UPMC's clinical research, implementation science and data analysis, with a particular emphasis on UPMC's learning health system initiatives. He also is associate vice chancellor for health care innovation for the Schools of the Health Sciences at Pitt. He is a distinguished professor and holds the Mitchell P. Fink Endowed Chair in Critical Care Medicine at the University of Pittsburgh, with secondary appointments in medicine, health policy and management, and clinical and translational science. Since 2008, Angus has served as chair of the Department of Critical Care Medicine. Since 2015, he also has been the physician director of the UPMC ICU Service Center, responsible for the provision of ICU services across the 30-plus hospital system. He also is a senior editor at JAMA.
Angus is a world-renowned clinical, translational and health services researcher. His research interests include clinical, epidemiologic and translational studies of sepsis, pneumonia and multisystem organ failure as well as health services research of the organization and delivery of critical care services. He is a leader in developing and evaluating approaches to facilitate smarter decision making and faster learning in health care, including novel Bayesian adaptive platform trial designs, the application of machine learning to large-scale data, and the use of behavioral economics and decision psychology to support optimal decision making. He has led numerous NIH-funded multicenter studies, written several hundred papers and is a Clarivate Highly Cited Researcher.
A fellow of the Royal College of Physicians of the United Kingdom, he has received multiple national and international honors, including election to the American College of Physicians, Honorary Lifetime Membership of the European Society of Intensive Care Medicine, Distinguished Research Award of the Society of Critical Care Medicine, and introduction into the inaugural class of Masters of the American College of Critical Care Medicine. He completed medical school and internal medicine training at the University of Glasgow and affiliated teaching hospitals, and he completed a fellowship in Critical Care Medicine and his MPH in Health Services Administration at the University of Pittsburgh.
- 2021 - Successes in Telemedicine - Caring for Patients at Home Part of the Dr. Loren Roth Speaker Series of UPMC
Successes in Telemedicine - Caring for Patients at Home Part of the Dr. Loren Roth Speaker Series of UPMC
Tuesday, March 23, 1-2:30 P.M.
Virtual via ZoomKeynote Speaker

Joseph C. Kvedar, MD
Chair of the Board, American Telemedicine Association
Professor, Harvard Medical School
Senior Advisor, Virtual Care, Mass General Brigham
Editor, npj Digital MagazineAlso featuring:
Richard J. Wadas, MD, FACEP, FAEMS
Executive Vice Chair, Community Emergency Medicine
Senior Medical Director, Center for Community Hospital Medicine
Medical Director, Office of Referring Physician Relations/MedCall
Clinical Professor of Emergency Medicine, University of Pittsburgh School of MedicineRobert Bart, MD
Chief Medical Information Officer, UPMCAbout the Speaker
At Mass General Brigham (formerly Partners HealthCare), Dr. Joe Kvedar has focused on driving innovation, creating the market, and gaining acceptance for connected health for nearly three decades. He is now applying his expertise, insights, and influence to advancing adoption of telehealth and virtual care technologies at the national level. Dr. Kvedar continues to guide the transformation of healthcare delivery as a respected thought leader, author, and convener.
Dr. Kvedar is Chair of the Board of the American Telemedicine Association (ATA). As Editor-in-Chief of npj Digital Medicine, a Nature Research journal, he is working to establish the evidence base needed to guide innovation and the implementation of virtual care.
He is co-chair the American Medical Association's (AMA) Digital Medicine Payment Advisory Group (DMPAG), which works to ensure widespread coverage of telehealth and remote patient monitoring, and successfully established several new provider codes for telehealth reimbursement through the CPT process. Dr. Kvedar is also a member of the AAMC’s (Association of American Medical Colleges) telehealth committee, creating tools that will enable medical schools and residency programs to integrate telehealth into the training of future practitioners.
Dr. Kvedar is the author of two books: The Internet of Healthy Things and The New Mobile Age: How Technology Will Extend the Healthspan and Optimize the Lifespan. The cHealth Blog provides his insights and vision for connected health.
Dr. Kvedar is a Professor of Dermatology at Harvard Medical School.
Connect on Twitter @jkvedar
Connect on Linkedin
- 2020 - Allan Frankel, Managing Partner for Safe and Reliable Healthcare
Monday, February 10, 1-3:30 P.M.
University Club, Ballroom B
123 University Place
Pittsburgh, PA 15260Keynote Speaker
Allan Frankel, Managing Partner for Safe and Reliable Healthcare
View Webcast »About the Speaker
Allan Frankel is a globally recognized high reliability expert with a deep focus on leadership and culture change. He also serves as senior faculty for the IHI and Intermountain Advanced Training Program. He has worked with organizations such as The Joint Commission, authored many peer-reviewed publications, co-developed many survey instruments for the U.S. and other countries, and continues to serve as senior advisor for reliability for organizations such as the Military Health System, Kaiser Permanente, Mayo Clinic, and several leading health systems.
- Previous Sonis Lecture Speakers and Topics
2017 - “Restoring Public Trust in Professional Self-Regulation"
Thomas H. Gallagher, professor in the Department of Medicine and the Department of Bioethics and Humanities, University of Washington2015 - "Palliative Care Futurist: Matching Care to Our Patient’s Needs"
Diane E. Meier, director, Center to Advance Palliative Care; co-director, Patty and Jay Baker Palliative Care National Center; Catherine Gaisman Professor of Medical Ethics; vice-chair for public policy and professor; Department of Geriatrics and Palliative Medicine, Icahn School of Medicine at Mount Sinai; New York, N.Y.2014 - “Learning Organizations, Implementation Science and Quality Improvement: Health Services Research at the Crossroads”
Lisa V. Rubenstein, professor of medicine and public health, VA of Greater Los Angeles and UCLA; director, Center for Implementation Practice and Research Support, senior scientist, RAND, Los Angeles, California2013 - "Will Equity Be Achieved Through Health Care Reform?"
John Ayanian, collegiate professor of internal medicine, professor of health management and policy, professor of health policy; director, Institute for Healthcare Policy and Innovation, University if Michigan, Ann Arbor, Michigan2012 - "The Affordable Care Act and the Broken U.S. Healthcare Delivery System: Strong Medicine or Placebo?"
Ashish Jha, associate professor of health policy and management, Harvard School of Public Health, Boston, Massachusetts2011 - "Comparative Effectiveness Research: The Essentials"
Harold C. Sox, professor of medicine, Dartmouth Institute for Health Policy and Clinical Practice, Dartmouth Medical School, Hanover, New Hampshire; editor emeritus, Annals of Internal Medicine2010 - "Tilting at Windmills: The Quest for Health Reform"
Elizabeth A. McGlynn, associate director, RAND Health, RAND Corporation, Santa Monica, California2009 - "Chaos and Organization in Healthcare"
Thomas Lee, network president, Partners HealthCare, Boston, Massachusetts2008 - "Health Care: Solutions without Borders"
Karen Davis, president of The Commonwealth Fund, New York, N.Y.2007 - "Making Tomorrow's Vision Today's Reality: Improving Patient Safety through Value-Based Health Care"
Carolyn M. Clancy, director of the Agency for Healthcare and Research Quality, U.S. Department of Health and Human Services, Rockville, Maryland2006 - "Safe, Effective, Efficient, and Compassionate Health Care Without the Need for an Advocate"
Jonathan B. Perlin, undersecretary for health, Department of Veteran Affairs, Veterans Health Administration, Washington, D.C.2005 - "What It Will Really Take to Improve Our Nation's Health System"
Stephen M. Shortell, dean, School of Public Health, and Blue Cross of California Distinguished Professor of Health Policy and Management, University of California, Berkeley2003 - "The Geology of the Quality Chasm"
Edward Wagner, director of W.A. MacColl Institute for Healthcare Innovation; professor of public health and community medicine, University of Washington, Seattle2002 - "Money, Medicine, and the Physician-Patient Relationship"
Wendy Levinson, professor of medicine, University of Toronto, Ontario, Canada2001 - "Descent into Hell: Understanding Quality of Life in Cancer from the Researcher-Patient's Perspective"
William M. Tierney, professor of medicine and chief of the Division of General Internal Medicine and Geriatrics, Indiana University School of Medicine; senior research scientist, Regenstrief Institute for Health Care, Indianapolis, Indiana2000 - "Drug Safety: How Big a Problem? What Can Be Done?"
David W. Bates, professor of medicine, Harvard Medical School; chief of the Division of General Medicine, Brigham and Women's Hospital, Boston, Massachusetts1999 - "Quality of Health Care: Where Will It Be in the Next Century?"
Robert H. Brook, director, RAND Health Sciences Program, Santa Monica, California1998 - "Improving Physicians' Clinical Decisions: Art or Science?"
Stephen B. Soumerai, associate professor of ambulatory care and prevention, Harvard Medical School, Boston, Massachusetts1997 - "Quality of Health Care: Where Will It Be in the Next Century?"
Robert H. Brook, director, RAND Health Sciences Program, Santa Monica, California1996 - "Medical Injury, Malpractice Litigation, and the Cost of Health Care in the United States"
Troyen E. Brennan, professor of medicine, law, and public health, Harvard Medical School and Harvard School of Public Health, Boston, Massachusetts1995 - Irwing Redlener, MD
1990's Inaugural Lecture by C. Everette Koop, Surgeon General of the U.S. 1982-1989

